Integrated Nutritional Theory with Traditional Chinese Medicine for Diabetes
by Walter Campbell, DAOM, A.P.
Foreword
It is commonly accepted that the future of Alternative Medicine is to work directly with conventional Western Medicine toward an integrated system. Unfortunately, this “integrated” approach places pressure on the TCM physician to adapt our art to help the patient simply manage the side effects of Western drugs. Nonetheless, there are many cases in which we should integrate with Western Medicine. The gap between TCM and Western Allopathic Medicine is filled with well-researched Alternative Medicine that can be integrated within the TCM Model. Refusal to incorporate some basic, well-researched nutritional supplements in our practice is as irresponsible as the shortsightedness of traditional Western medicine. Many patients suffer needlessly because the TCM Physician will not consider treatments beyond the scope of TCM, a myopia that has thwarted the advancement of medicine since its inception.
The amount of energy spent to incorporate TCM with Western Allopathic Medicine should at least be matched with learning other alternative disciplines such as integrated nutrition, in addition to understanding blood work and how it can relate to TCM and nutrition, as well as the naturopathic philosophy of health, especially in terms of colonic health, Reiki, and its relationship to Qi Gong. These disciplines, among others, can help us treat the patient using TCM with new insight to create a parallel protocol with a deeper understanding of disease.
Introduction
One shortcoming of integrating TCM with Naturopathic Medicine is that we lack a complete picture, a real dynamic model of the systems involved. A Chinese Medicine myth maintains that the Zang Fu organs are not real but are functional symbols to account for the patterns involved. What we need is a Rosetta stone that translates Chinese Zang Fu organ function into a real working functional physical model in terms of Western Medical Theory. If, for instance, the liver is overacting on the spleen according to the Five-Element diagram of the systems, how does that pattern translate into the actual organs in terms of Western medicine? Developing a common working integrated model of both systems is not only critical to using nutritional supplements with Chinese Medicine but will provide insight into a better logistical pattern and protocol.
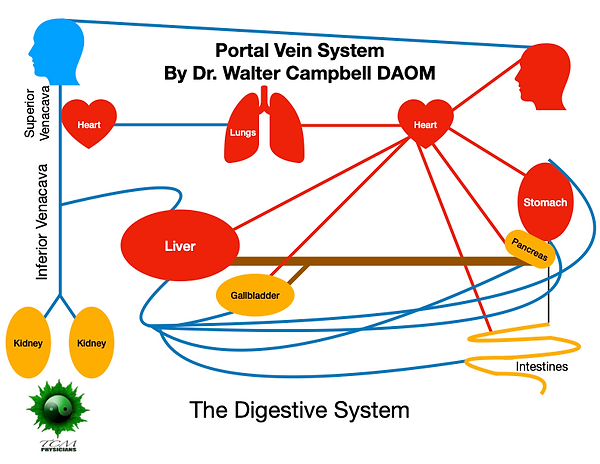
The Portal Vein System
The portal vein system is a complete subset system separate from the rest of the circulatory system. Only the organs used for digestion (the gallbladder, pancreas, stomach, and intestines) pipe blood through the portal vein system into the liver. (The only exception may be the spleen, which is included in the portal vein system, unless we consider the spleen as an organ that digests old blood cells for reprocessing through the liver via the portal vein system, in which case it is more aptly considered a digestive organ). Most important, blood circulation to these organs depends on how much blood goes through the liver. The implications of a liver depression in TCM terms and of blood going through the portal vein system form the heart of this model.
The symptoms of bile stasis and the resulting mild portal vein hypertension correlate with the differentiating syndromes according to the Sanjiao Theory.
Since the liver is a filter, it needs a waste disposal system. A healthy liver filters approximately two quarts of blood per minute. When the liver is congested or depressed as a result of alcohol use or bad diet, the blood flow through the liver can be reduced to one-tenth (or even less with more serious conditions such as hepatitis). A depressed liver can lock up thirty to fifty percent of the total blood in the body in the portal vein system. Such grand-scale blood stagnation and vacuity have dire consequences. The resulting backpressure on the radial artery from portal vein hypertension, I believe, is one of the main contributing factors to the hardened feel of a wiry pulse.
The liver acts as a major processing plant to dispose of the waste that it filters from the blood. In most naturopathic models, this process is broken down into two parts: Phase One breaks down waste products into smaller pieces. Phase Two either: 1) directs these pieces through the bile tract, which leads to and past the gallbladder into the common duct, where the pancreas discharges its alkaline juices and digestive enzymes into the small intestine, or 2) directs the waste to the kidneys to be discharged in the urine. Frequent urination tends to accompany a depressed liver because of the overload from the liver being directed to the kidneys.
This same mechanism occurs with too much glucose in the blood. If the liver cannot take in glucose, either because the pancreas is not producing enough insulin or because of insulin resistance, the kidneys are left to excrete the excess glucose. The muscles, liver, and brain use most of the glucose, but one cannot help but wonder: What happens when the liver is congested, when the liver’s phase two is backed up (called liver qi stagnation, or liver depression)? Can liver depression have such a negative effect on the liver cells that they develop insulin resistance? That is, can the liver cell membrane become so compromised from oxidative stress that the docking stations for insulin not only prevent the insulin from hooking up with the cell membrane but also prevent glucose from entering the cell? If this is the case, addressing liver depression would benefit glucose levels in a diabetic, as I have found in my practice. The most significant effect I have observed is the reduction of the amount of insulin needed by insulin-dependent diabetics.
Bile Stasis
The bile tract from the liver to the small intestine is curtailed by bile oversaturated with metabolic waste from a depressed liver, a major concept in naturopathic medicine. This saturation slows down the liver’s ability to detoxify itself, and with increased liver depression comes decreased blood flow through the digestive organs. The pancreas suffers significant trauma in a number of ways: The blood supply through the portal vein system slows because the liver filters the blood on the first pass. I believe that this syndrome is common to syndrome x with yin vacuity and can affect the quality of insulin made by the pancreas. The common duct can become blocked or curtailed with toxic bile, putting stress on the pancreas to make and/or deliver digestive enzymes and alkaline juices to the small intestine. With little or no digestive enzymes, the food entering the small intestine from the stomach is not digested completely. With little or no alkaline juices, stomach acid is not completely neutralized. As a result, stomach acid is reabsorbed through the portal vein and returns to the liver, a catch-22 that creates an imbalance in the body. Naturopaths call this imbalance systemic acidosis.
Combine this with ketoacidosis, in which the body cannot process sugar properly and excess fatty acids released from the digestion of fat throughout the body are converted by the liver into chemical compounds called ketones. As ketones enter the bloodstream, they cause the blood to become dangerously acidic, and with acid come corrupted cell membranes and stagnation of fluid and yin vacuity, or dryness.
Systemic acidosis among diabetics is a major contributing factor in:
- Degeneration of the eye
- Neuropathy of the feet
- Insulin resistance due to degeneration of the cell membrane
Acidosis causes inflammation, slowing the circulation and increasing inflammation. The damage to the capillary beds (lipid peroxidation in the cell membrane) becomes extensive, especially in the feet, causing edema and neuropathy. In addition, an excess of acid and lack of digestive enzymes significantly increase the potential for irritable bowel syndrome as undigested food and unbuffered acid travel down the digestive system.
One sign of systemic acidosis, though not in every case, is acid reflux. When the liver is acidic, the two valves entering and leaving the stomach freeze open. The allopathic protocol for acid reflux is to prescribe a drug to prevent the stomach from making acid or to buffer stomach acid. This drug prevents the common duct from opening because there is not enough acid to trigger the opening of the common duct. Blockage of the common duct prevents the liver from detoxifying, and while there is not enough acid to open the common duct, a significant amount of acid is still discharged from the stomach into the small intestine then reabsorbed by the portal vein system back to the liver. While this amount of acid is small, the cumulative acidic buildup in the system in a significant number of cases renders antacids useless. Most critically, a patient on antacids for an extended length of time is in a major induced state of bile stasis. Why does the allopathic model have acid building up only in the lungs and kidneys but never in the liver?
Returning the pH to normal eliminates most cases of acid reflux. Prescribing an alkaline diet and/or an enteric-coated Sodium Bicarbonated and Potassium Bicarbonated pill usually alkalinizes the liver and stops acid reflux in about a week. The enteric-coated pill dissolves in the small intestine; the bicarbonates are absorbed by the small intestine, move into the portal vein, and are then transported directly to the liver.
Alkalife, the maker of Bicarb Balance, makes other natural products that alkalinize the patient’s blood, usually within a week. A simple litmus test of the pH of the urine and saliva quickly reveals whether the physician’s protocol is raising the pH.
I have successfully treated eight out of ten cases of acid reflux, including severe ones in which conventional medicine had yielded no results. Using bicarbonates for acidosis is easier on the patient while using herbs and acupuncture to resolve the pattern. I recommend one tablet of Bicarb Balance with breakfast and dinner for mild cases or two pills with every meal (not to exceed six pills per day) for difficult cases.
Acid reflux is defined as liver overacting on the stomach, but I believe that it is really the liver overacting on the spleen. Most TCM physicians agree that the TCM spleen has been misnamed. When translated correctly, the TCM “spleen” should be called the TCM pancreas. Considering naturopaths’ constructs and those of TCM, acid reflux may actually be the liver overacting on the pancreas.
According to JAMA (Dec. 27, 2006, Vol. 296, No. 24), patients who had been taking antacid drugs for over four years experienced a 59% increase in hip fractures. As naturopaths maintain, antacids not only interfere with the absorption of minerals by reducing stomach acid but help to melt bone mass as the body steals calcium from the bones to neutralize the acid in the blood.
Stresses on the Diabetic Pancreas
The pancreas is a vital organ, producing:
- Insulin
- Alkaline juices
- Digestive enzymes
If the pancreas struggles to deliver alkaline juices and digestive enzymes and the liver is depressed because of bile stasis (which may restrict blood flow through the portal vein system from the pancreas), it follows that the pancreas would have trouble producing insulin.
In TCM, the terms that describe such patterns are: heat and damp, toxic damp heat, and damp heat with yin vacuity, the last being the most common at the end of the cycle. Sometimes the heat starts as an exogenous pathogen beginning in the liver, which causes damp heat in the gallbladder; or, the heat may start as dryness in the lung, which congests the spleen with dampness, eventually causing the qi to knot (or stagnate) in the liver, creating heat and leading to damp heat in the liver. In cases of liver blood vacuity, lung heat dries the moisture, then stomach fire dries the middle, followed by frequent urination.
It is essential for the TCM physician to understand these patterns. While we may debate the patterns and the progression of the patterns during treatment, correlating the pressures on the diabetic pancreas with TCM patterns helps us to establish a more effective patient protocol. We know that the wasting, thirsting, and hence dryness of the upper, middle, and lower Jiao are the central causes of diabetes in TCM. But, do we consider this same dryness, which causes the bile to dry out and stagnate bile (bile stasis), a key determinant of the health of the pancreas?
The herb Chi Hu in a formula effectively treats liver depression. One of its chief actions is the increased production of bile in the liver. Chi Hu is very drying and can actually worsen the patient’s symptoms by trying to push new bile into a clogged system. Chi Hu helps to break up bile stasis by producing new bile, an action that I believe is paramount in treating diabetes. Biotic Research has a product called Beta Plus, which, while not a Chinese formula, is specifically formulated to treat bile stasis and can break it up in most cases in ten to thirty days. Once bile stasis is eliminated, the patient can use a Chi Hu formula. Bile stasis is not a Chinese pattern, but understanding it can help TCM physicians to relieve pressure on the pancreas and liver. Beta Plus is made from beet extract, digestive enzymes, and ox bile.
Glucose Tolerance Factors
As naturopaths maintain, glucose tolerance factors (GTFs) are the prime limiting factors needed by the pancreas to make insulin and in the metabolism of glucose and carbohydrates. Accordingly, every health food store in the United States has GTF products from various vitamin companies. Specifically, chromium and vanadium are some of the prime limiting factors that the pancreas uses to make insulin. Some studies suggest that vanadium can act like insulin in triggering the cells to take in glucose. Other GTFs are niacin, niacinamide, biotin, vitamin B6, copper, magnesium, zinc, and vitamin C. Helpful herbs include cinnamon, bitter melon, and American ginseng. Useful Ayurvedic herbs are Amla, Gymnema Sylvestre, Neem, Pata de Vaca, and Salacia Oblonga.
Chromium
The effect of chromium on glucose metabolism apparently requires its conversion to GTF, a low-molecular-weight compound that contains chromium, niacin (nicotinic acid), glycine, glutamic acid, and cysteine. GTE has been shown to potentiate the action of insulin at the cellular level.1.4
Tissue chromium levels were found to decline with age in Americans.2 In other studies, including one by the U.S. Department of Agriculture, more than 50% of people consumed less than the lower level of chromium recommended by the National Academy of Sciences, Nutritional Research Council.3,37 Chromium aspartate is a well-utilized form of supplemental chromium being solubilized at a wide range of pH. The amounts of chromium used in most clinical trials (*150 to 200 ug/day) are apparently inadequate for some patients, even when more efficient chromium compounds are used. Larger amounts of chromium, such as 500 to 1,O00 ug/day, have often had a greater benefit.4
Niacin and Niacinamide
As a component of glucose tolerance factor, niacin plays an important role in carbohydrate metabolism. Many refined foods consumed by Americans are depleted of niacin. Grains and other foods that are “enriched” usually contain added niacinamide, which apparently cannot be converted by the human body into niacin. In addition, many vitamin supplements contain niacinamide rather than niacin. Although niacinamide can perform most of the functions of vitamin B3, a small amount of niacin seems to be necessary for the synthesis of GTF.5 Both niacin and niacinamide may also be important for blood sugar control through a mechanism unrelated to GTF. As precursors to NAD, an important metabolite concerned with intracellular energy production, niacin and niacinamide may prevent the depletion of NAD in pancreatic B cells.
Biotin
The initial step in glucose utilization by the cell is its phosphorylation, mediated by the biotin-dependent enzyme hepatic gIucokinase. Thus, adequate biotin intake is required to initiate intracellular glucose into the cell.6
Biotin may also play a role in stabilizing blood sugar levels through biotin-dependent enzymes acetyl Co A carboxylase and pyruvate carboxylase.37 Thus biotin deficiency should be avoided in those with blood sugar disorders.
Pyridoxine (vitamin B6)
Serum vitamin B6 levels were below normal in 25% of 5I8 diabetics.7 Particularly where peripheral neuropathy is present, the inadequate B6 intake should be contemplated.8
Copper
Because the typical American diet contains only about half of the RDA (2mg/day) for copper.9,36 deficiency of this mineral may be common. Copper is involved with insulin binding, and copper deficiency in mammals may be reflected in increased glucosylated hemoglobin, indicative of chronically raised blood sugar levels.10
Magnesium
The American diet is often low in magnesium. Dietary surveys have shown that 80-85% of American women consume less than the RDA for the mineral.11 Daily magnesium intake in two other studies was only about two-thirds of the RDA.12,13,36 This may be particularly relevant in diabetics, where magnesium deficiency is thought to play a role in the development of insulin resistance.14 Serum magnesium has been found to be significantly lower in many diabetics,15 therefore it is reasonable to make sure that diabetics have adequate dietary intake of magnesium. Low magnesium levels may also be associated with hypoglycemia.16
Zinc
Zinc is involved both with insulin synthesis by pancreatic B cells17 and insulin binding to liver and adipose tissue cells.18,19 People with zinc deficiency may have significantly higher glucose levels and lower insulin levels than similar patients without zinc deficiency.20
Vitamin C (ascorbic acid)
Ascorbic acid levels may be lower in diabetics than controls,22 and patients with inadequate ascorbic acid levels may be found to have abnormal blood sugar curves.23 In addition. ascorbic acid may compete with glucose for transport across cell membranes,24 so that in hyperglycemia, ascorbic acid transport into the cell may be inhibited.25
Ascorbic acid deficiency may allow sorbitol to accumulate in erythrocytes, which may pre-dispose diabetics to certain types of end-organ damage.26 Care should be taken to ensure that those with blood sugar abnormalities have adequate ascorbic acid intake.
Manganese
Manganese is a cofactor for certain enzymes involved in the intermediary metabolism of carbohydrates. In addition, the concentration of manganese in the pancreas is approximately ten times higher than in other organs.27
The optimal intake of manganese is not known but at least half of the manganese is lost when whole grains are replaced by refined flour.29 The American diet may be low in manganese.3
Both B12 and folate are involved in a number of different steps in carbohydrate metabolism and the incidence of B12 deficiency was significantly greater in a series of diabetics than in the general population.30 Folate is involved with gluconeogenesis as a cofactor with key enzymes in the liver and small intestine.31 Deficiency of either B12 or folate is to be avoided in those with blood sugar abnormalities.
Vitamin B1 (thiamin)
Central to carbohydrate metabolism and Krebs Cycle function is adequate thiamin levels, and diabetics are more often deficient in thiamin.32 Care should be taken to ensure that thiamin intake is adequate in those with diabetes and hypoglycemia.
Carnitine
Carnitine is involved as part of a vital transport mechanism of fat metabolism in which fat enters the energy production pathway. Carnitine supplementation may be considered in those with blood sugar abnormalities.
Vanadium
Vanadate is an oxidized form of vanadium. Due to possible insulinotropic effects of vanadate33, inadequate amounts of this trace mineral is undesirable in those with blood sugar abnormalities.
Vitamin E and Selenium
Vitamin E and selenium are essential nutritional factors which act as antioxidants and may be involved in glucose balance.34,35 Since many complications associated with diabetes may be related to excess free radical activity, prudence demands that adequate selenium and vitamin E be supplied in the diabetic diet.
The minerals listed above are severely lacking in U.S. agricultural soils. Food grown in the U.S. is void of many trace minerals because most crops are grown year after year in the same soil. For the most part the farmer only replaces nitrogen phosphorus potassium with a little boron. Without these trace minerals the pancreas makes weak insulin and the cells demand more insulin, further depleting the body’s reserves of these minerals. This cycle continues until the pancreas fails. Veterinarians in the 1930s discovered that livestock deprived of chromium and vanadium suffered from diabetes, so they enriched the feed with chromium and vanadium to protect the livestock against diabetes. Naturopaths as well as homeopaths have used these trace minerals to treat diabetes for over fifty years.
Cinnamon
Data from the Agricultural Research Unit in Maryland, first published in the New Scientist in August 2000, showed that cinnamon rekindled the ability of fat cells in diabetics to respond to insulin and greatly increased glucose removal. It is believed that a substance in cinnamon called MHCP is the main reason for its beneficial results.
The researchers recommend that type II diabetics should take a quarter to one full teaspoon of cinnamon per day.
The insulin resistance that leads to type II diabetes develops relatively slowly as the body ages and even those who have not yet experienced severe symptoms may have some degree of elevated insulin resistance.
Cinnamon is also a rich source of magnesium, which is essential for maintaining bone density, electrolyte balance, certain enzyme functions and many other crucial biochemical processes. Magnesium is also linked to the more dramatic forms of diabetes that occur earlier in life.
Amla
Amla is one of the richest natural sources of Vitamin C and naturally occurring bioflavonoids; it contains 30 times the amount of Vitamin C found in oranges. It is a powerful antioxidant that cleanses and revitalizes; the entire system regulates blood sugar and prevents lipid peroxidation in cell membranes.
Gymnema Sylvestre
Gymnema Sylvestre leaves raise insulin levels, according to research in healthy volunteers. Based on animal studies, this may be due to regeneration of the cells in the pancreas that secrete insulin, or by increasing the flow of insulin from these cells. Other animal research shows that gymnema can also reduce glucose absorption from the intestine, improve uptake of glucose into cells, and reducing blood sugar levels.
Bitter Melon
Bitter Melon has been shown to lower blood glucose levels in scientific studies in animals and humans. At least three different groups of constituents in Bitter Melon have been reported to benefit diabetics. These include a mixture of steroidal saponins known as charantin, insulin-like peptides, and alkaloids. Bitter Melon has been shown to significantly improve glucose tolerance without increasing blood insulin levels, and to improve fasting blood glucose levels.
Neem
Neem was first mentioned in India’s ancient Ayurvedic Medical texts. This medicinal information about Neem was spoken about in the Vedas, the world’s oldest books [over 5000 years old). At least 100 bioactive substances have been found in Neem, including nimbidin, azadiracthins, and other triterpenoids and limonoids. It has been scientifically shown to be effective in treating diabetes.
Research papers on Neem have been written by many institutions in the U.S. and abroad: Murty, 1978; Chakrabartty, 1984; El-Harwary, 1990; Pillai, 1931; and Luscombe, 1974, to name a few.
American Ginseng
American Ginseng is an herbal medicine used to increase physical and mental well-being. It may also be used to treat high blood sugar. One study found that people with type-2 (adult-onset) diabetes who took American ginseng before or in conjunction with a high sugar load experienced less of a rise in blood glucose levels.
Pata de Vaca
Pata de vaca’s use as a natural insulin substitute was confirmed in two Brazilian studies, conducted by two separate research groups. Both studies reported En vivo hypoglycemic actions in various animal and human models. Chilean research in 1999 reported the actions of pata de vaca in diabetic rats. Their study determined that pata de vaca was found to “elicit remarkable hypoglycemic effects” and brought about a “decrease of glycemia.”
Salacia Oblonga
Salacia Oblonga studies indicate that ingestion of the herb lowers insulin and blood sugar levels. Steve Hertzler, Assistant Professor of nutrition at Ohio State University, said the effects of the Indian herb are similar to what would be seen with prescription medications. In a study conducted by Kowsalya et al, it was determined that Salacia Oblonga was effective in lowering blood glucose, serum cholesterol and triglycerides, and in increasing the HDL cholesterol levels of non-insulin-dependent diabetics.
In a TCM diabetic patient, the physician can tweak patterns endlessly and provide the best formulae and acupuncture to fit the patterns, but if the patient suffers from GTF depletion, success will be marginal at best. Diabetic patients must be provided with glucose tolerance factors in addition to herbs and acupuncture. A patient whose fasting levels of glucose and triglycerides are high is likely pre-diabetic; this patient, too, should be prescribed glucose tolerance factors along with treating the pattern, and the physician should be mindful of bile stasis.
Future Study for the New Diabetic Clinic
Patients whose blood work indicates that they are pre-diabetic should be broken into two groups: the first group treated with herbs and acupuncture alone; the second group with herbs, acupuncture, and a GTF formula. Blood work should be conducted at the onset of the study before and after thirty days of the protocol. The evidence would be in the group with the best blood work.
Summary
Diabetes may be caused or exacerbated by bile stasis, which can lead to liver depression, which in turn affects blood flow to the spleen, gallbladder, pancreas, and intestines. The decrease in blood flow to the pancreas affects its ability to make insulin. Excessive blockage impedes the pancreas’s ability to discharge its alkaline juices and digestive enzymes through the common duct.
Decreasing blood flow through the portal vein system to other digestive organs causes a variety of ailments:
Organ suffering from decreased circulation effects
Stomach Acid reflux
Stomach ache
Gallbladder Thickened walls
Gallstones
Intestines Constipation,
Irritable bowel syndrome
Hemorrhoids
Spleen (Western) Blood vacuity
The Kidneys
If portal vein hypertension is blocking a significant amount of blood in the portal vein system, say 30%, from the rest of the circulatory system, the heart still attempts to put out 100% (in a 70% system), which contributes to high blood pressure. The combination of high blood pressure and systemic acidosis is the primary cause of kidney failure. According to the naturopathic saying, “You can only cook a stone in the gall bladder and/or the kidney when the blood is acidic.”
Depression
The neurotransmitters are made in the small intestine. If the bile is toxic enough and pushed through the common duct, could the toxic bile be absorbed by the small intestine and affect the production of neurotransmitters? If phases one and two are backed up in the liver and the liver cannot filter all the toxins out of the blood on the first pass, could either one of these mechanisms affect the patient’s shen?
Given the same mechanisms, could the heart pull enough blood through the system to feed the brain? When the heart goes into a very slow alpha rhythm during sleep, will the brain wake the patient up with a bad dream to get his heart going? Will the brain keep the patient awake because the heart cannot pull enough blood through the liver to feed the brain? Taking a sleep aid such as Tylenol P.M. (which can depress the liver even more) puts the patient asleep neurologically. Can this affect the patient’s memory? Could any of this contribute to a patient’s anxiety?
It would be interesting to match TCM patterns with some of the syndromes mentioned above. TCM has known for years about the heart and liver working with the mind or shen, where we have the invasion of the liver by an exogenous factor disturbing the liver qi and working against the gallbladder qi, constriction of chest and/or phlegm misting the heart and disturbing the shen. The question is: Can we construct a physical picture that would account for the TCM model? Does the heart have to work harder to suck blood through a congested liver? Can toxic bile corrupt neurotransmitters that are being made in the small intestine?
We always label the pattern as if it were fine art, which is important, but what does that really mean in terms of the actual pathology in the patient? The inability to correlate the pattern with physical pathology leaves us at a major disadvantage.
Exercise and Diet
An alkaline diet and moving the blood through exercise are crucial to the diabetic’s prognosis.
Sugar substitutes commonly found in diabetics’ diets only exacerbate the disease: Diet Coke, for example, contains an excess of phosphoric acid and is a strong diuretic, a combination conducive to acidosis. Aspartame and Splenda are not safe for man or beast; only Stevia should be used as an artificial sweetener.
Dr. Joanna Budwig’s Protocol
A brilliant scientist who studied fats for the German government analyzed the composition of the cell membrane through the electron in 1945. One of her major conclusions was that the cell membrane was in charge of the day-to-day operation of the cell, not the nucleus. It is imperative to keep the docking stations on the cell membrane from oxidative stress. Corruption of the membrane prevents the insulin, thyroid, and every other hormone from dropping off their software.
Budwig’s major contributions include her findings that trans-fatty acids not only corrupt the cell membrane but that the cells could not digest the trans fats (because all the valence electrons had been stripped away in processing, leaving the trans fat metabolically dead in the cell. That is, there were no chemical handles on the trans fat for the cell to grab and metabolize).
She asked herself the questions: How do I rebuild the cell membrane? How do I digest the trans fat?
Answer: Find an oil rich in Alpha Linoleic Acid and add some sulfur-based amino acids, the main constituents of the cell membrane, and find a way to add electrons to the system. This would rebuild the membrane.
Solution: Flaxseed Oil, 58% Alpha Linoleic and extremely rich in excess electrons, and cottage cheese, rich in sulfur-based amino acids. Mixing the two yields a water-soluble oil that quickly diffuses through the body and into and through the cell membrane, effectively repairing the cell membrane.
Supply the excess electrons to dissolve the trans fatty deposits in the cell. Repairing the cell membrane in the diabetic patient is critical.
Formula:
Mix in a blender:
- 14 Tablespoons of flax seed oil
- 1 pound of cottage cheese.
- 1 cup of water
Take 3 tablespoons of this mixture per day.
Enzyme Therapy
I have used enzyme therapy in my practice for diabetic patients, provided they were not taking any blood thinners. Following is a concise article about enzymes by Dr. William Wong.
Treating Diabetes With Enzymes: What We Know Now
By Dr. William Wong, ND, PhD
Up to a year ago, for anyone asking if systemic enzymes could help lessen the load of troubles that beset Type 1 diabetic patients, I would have told them about lowering pancreatic inflammation, and possibly helping with lower extremity circulatory issues. I would have never suggested that the use of enzymes could decrease the need for insulin, increase energy or reverse the seemingly myriad of things diabetics suffer from. Then we started getting information from Type 1 patients that amazed even me and that have subsequently sparked new research. Here are two typical case histories.
Case History #1:
A Type 1 diabetic Native American patient from Montana in his mid 40’s, very insulin dependent, with peripheral neuropathy in the lower extremities (LE’s) and presenting paresthesia as well in the upper extremities (UE’s) radiating distally to the hand. Peripheral Vascular Disease (PVD) in the LE’s had already caused several toes to be amputated.
Patient began taking therapeutic doses of fibrinolytic systemic enzymes. Within weeks, circulation was opened in his feet and lower extremities. Skin there returned to a pink / flesh color. Remaining toes now have full circulation and are no longer candidates for amputation. Lower extremity and upper extremity pain became paresthesia (tingling and pins and needles), and as a result is much more bearable.
The patient’s insulin needs were decreased.
Case History #2:
86-year-old male Caucasian from Las Vegas history of Type 1 Diabetes for over 50 years. One below the knee amputation (left side) already done due to DVP, the other leg about to be amputated due to general lack of blood flow and arterial blockage. Poor circulation body wide and a gray / white pallor to the skin also body wide. Neurological pain was had at both lower extremities. Urine flow beginning to flag as patients kidneys became laden with scar tissue (Glomerulosclerosis). Patient was highly insulin dependent. Above that the patient was functionally blind in one eye from a Lasix procedure that had generated scar tissue over the retina.
After several weeks of systemic enzyme use the patient first noticed a lessening in his lower extremity neurological pain (neuropathy). His skin color in the remaining leg changed to rosy as circulatory pathways were opening. Outer layer of whitish dead skin shed off leaving what resembled a “body wide dandruff”, exposing new pink /flesh tone skin beneath. The existing leg became pink with blood flow, no longer ulcered, no longer had ischemic pain and was saved from amputation.
Urine flow increased as fibrin was lysed (eaten away) from the kidneys. If the urine was allowed to stand in the toilet a layer of tiny bits of fibrin (component of scar tissue) in what resembled fiberglass floated to the top. The fibrosis that had blinded one eye was lysed away and the patient now has better than 20/20 vision in that eye. Most significantly, the patients own insulin production has returned (thought to be impossible under the auto immune theory of diabetic pancreatic destruction). He is no longer insulin dependent. After medical testing the patient is no longer considered diabetic at all and is off all medication.
Sound fantastic? It did to me, even as a Naturopath who expects nature to do fantastic things. Diabetes is one of those diseases you never expect patients to get better from. Even after several years of working with systemic enzymes I had heard of some Type 2 patients improving their energy and leveling off their sugar highs and lows but I had never expected any form of improvement in Type 1 patients, the medical literature was very clear. Once the immune system destroyed the insulin producing portions of the pancreas, there was no getting those tissues to function again! That medical “truth” has turned out to be merely a medical theory.
Lets take a look at the present understanding of the root causes of diabetes and add our own conjectures based on what we have observed clinically. We know from the present research work being done that the root cause of diabetes is inflammation of the pancreas. How and why this inflammation sets in we yet do not know. As we also know from the physiology of trauma, inflammation breeds fibrosis or scar tissue. One follows a chronic course of the other.
Fibrosis is also the culprit in the Peripheral Vascular Disease. In this condition, fibrin plugs form in the micro circulation (tiny blood vessels) forming blockages to full blood flow. Fibrin also forms the matrix for arterial plaque. Inflammation of trauma to the inner lining of an artery (intima), causes the traumatized or weakened section to shore itself up with scar tissue. On the spider web of scar tissue fat, calcium and heavy metals accrue forming what we know as arterial plaque. Once the fibrosis blockages become extensive enough, the patient presents the signs of PVD, which are cold extremities, intermittent caludication (pain on walking from lack of oxygen supply to the tissues known as ischemia), non healing ulcerations of the skin and eventual death of tissue creating gangrene leading to amputation.
The high blood sugar levels had during diabetes damages the body’s organs. One of the first organs to be damaged are the nerves to the legs and then the arms. Wherever the circulation is poorest the nerve damage follows and radiating nerve pain is had (neuropathy). The damage begins with, you guessed it, inflammation and progresses with, you guessed it again, fibrosis. It is this inflammation into fibrosis that seems to be a recurring theme in diabetes.
For a moment lets do some education on orally administered systemic enzymes. They have a 5 decade history of wide spread medical use in Germany, Central Europe and Japan with over 150 million patients in Europe alone having undergone enzyme therapy in the last 4 decades. There are over 200 peer-reviewed studies proving the absorption, therapeutic action and total lack of toxicity (no LD-50) of systemic enzymes. Their primary action is anti-inflammatory, (though not through a COX 1 or Cox 2 action. The enzymes instead “eat” pro inflammatory cytokines). The enzymes also have a proven lysing action on all types of fibrosis and scar tissue leaving normal or endogenous tissue entirely intact and un-bothered. This is due to the body “tagging” excesses of fibrin as exogenous proteins. (The subject of protein tagging and its discoverer won the Nobel Prize in biology in the late ’90’s). Entering the key words: systemic enzyme, serrapeptase, nattokinase, bromelain, pancreatin, papain, trypsin, chymo trypsin into the search engine at Pub Med will bring up some of the current research on systemic enzymes and their applications. A search in the “medical fields” section of www.mucos.cz will show abstracts of the extensive older research done with the first systemic enzyme blends of the 50’s and 60’s. It has to be said that there is nothing, no drug or substance, in either the allopathic medical world or in the natural health world that can remove scar tissue but highly fibrinolytic systemic enzymes.
Current thinking on diabetes is that the body’s immune system attacks the pancreas creating inflammation. This may be so. Further, the current thinking is that the inflammation brings about the destruction of the Islets of Langerhans and its Beta Cells, the places where insulin is made. This may not be so. If the studies that are currently being planned and executed further demonstrate what we are seeing clinically with Type 1 patients on systemic enzymes, then this point will have to be re-thought. Clinically most of the Type 1 patients have a significantly lower need for insulin while some no longer need the insulin at all. This would suggest that the Beta Cells and the Islets are not destroyed. I conjecture that they are merely clogged by the fibrosis created by the inflammation. Once the causative inflammation is reduced and once the fibrinolytic action of the enzymes has eaten away the fibrosis and reopened the channels, then what ever production the Islets can make can actually get into the system.
I believe that the global (body wide) non-toxic, anti-inflammatory effects of highly fibrinolytic systemic enzymes and the scar tissue eating effects of the same enzymes are the reasons we are seeing the decrease in pancreatic inflammation, decrease in diabetic neuropathy, in it’s associated Peripheral Vascular Disease, and the decrease in insulin dependence we are seeing clinically in Type 1 patients. Let’s see if the research further verifies the observed findings and gives us more insight into the pathways of action.
I have kept the degenerative effects of diabetes abated in senior citizens with this formula.
Side note: I believe that one day we will find that hormones not only drop off their software at the cell membrane but also carry a neurological charge that comes from the gland (comprised in part of neurological tissue) that created it. That is, every hormone comes with its own battery pack so that it can drop off not only its instructions but also energy to carry out the hormones’ commands. The energy is probably encoded with the command.
Areas for future research
If this is so, could insulin resistance be a failure of gland to impart a charge that is below cell membrane threshold? I was taught that T8 on the du channel is neurologically connected to the pancreas. If so, could acupuncture or even electrostim a T8 increase the charge threshold on the insulin?
Since the neurological connection to the gland comes from the brain, could the brain be sending corrupted software to the gland? Could the pancreas itself cause the corruption of the software, with one possible cause being blood stagnation caused by a congested liver in the portal vein system?
Does the brain have the ability to change the software in the hormone to fit the circumstance? If so, the insulin resistance may be a defense mechanism. Thus, 77% of the patients undergoing gastric bypass surgery who had diabetes before surgery have experienced complete remission a few months after the operation.
On the same note, diabetic patients who change their diet, work out, and lose the weight can go into complete remission. Self-image may play a part in reprogramming the software in the insulin.
References
Toepfer EW, Mertz W Polansky MM, Roginski EE,Wolf WR.
Preparation of chromium-containing material of glucose tolerance factor activity from brewers yeast extracts and by synthesis. J Agric Food Chem 1977;25:162-166.
Schroeder HA, Nason AP, Tipton IH.
Chromium deficiency as a factor in atherosclerosis. J Chronic Dis 1970;23: 123-142.
Anderson RA, Kozlovsky AS.
Chromium intake, absorption and excretion of subjects consuming self-selected diets. Am J Clin Nutri 1985;41:1 I77-1 183.
Glinsmann WH, Mertz W.
Effect of trivalent chromium on glucose tolerance. Metabolism 1966: 15:5 10,2.
Urberg M, Zemel MB.
Evidence for synergism between chromium and nicotinic acid in the control of glucose tolerance in elderly humans. Metabolism 1987;36:896-899.
Anonymous.
Biotin and glucokinase in the diabetic rat. Nutr Rev 1970;28:242-244.
Davis RE, Calder IS, Curnow DH.
Serum pyridoxal and folate concentrations in diabetics. Pathology 1976;8: 151-156.
Jone CL, Gonza1ex V.
Pyridoxine deficiency: a new factor in diabetic neuropathy. J. Am Podiatry Assoc 1978;68:646-653.
Wolf WR, Holden J, Greene FE.
Daily intake of zinc and copper from self selected diets. Fed Proc 1977;36:1175.
Klevay LM, Canfiedl WK, Gallagher SK, Henrickson LK, Bolonchuk W et al.
Diminished glucose tolerance in two men due to a diet low in ic acid in the control of glucose tolerance in elderly humans. Metabolism 1987;36;896-899.
Morgan KJ, Stampley GL, Zabik ME, Fischer DR.
Magnesium and calcium dietary intakes of the U.S. population. J Am Coll Nutr 1985;4:195-206.
Lakshmanan FL, Rao RB, Kim WW, Kelsay JL.
Magnesium intakes, balances and blood levels of adults consuming self-selected diets. Am J Clin Nutri 1984;40: 1380-1389.
Srivastava US, Nadeau MH, Gueneau L.
Mineral intakes of university students; magnesium content. Nutr Rep Int 1978:18;235-242.
Yainik CS, Smith RF, Hockaday TDR, Ward Nl.
Fasting plasma magnesium concentrations and glucose disposal in diabetes. Br Med J 1984:288:1027-1028.
Ceriello A, Guigliano D, Dello Russo P, Passariello N.
Hypomagnesemia in relation to diabetic retinopathy. Diabetes Care 1982:5:558-559.
Stebbing JB, Turner MO, Franz KB.
Reactive hypoglycemia and magnesium. Magnesium Bull 1982:2:131-134.
Emdin SO, Dodson GG, Cutfield JM, Cutfield SM.
Rose of zinc in insulin biosynthesis. Some possible zinc-insulin interactions in the pancreatic B-cell. Diabetologia1980;19:172-182.
Arquilla ER, Packer S, Tarmas W, Miyamoto S.
The effect of zinc on insulin metabolism. Endocrinology 1978; 103: 1440-1449.
Herington AC.
Effect of zinc on insulin binding to rat adipocytes and hepatic membranes and to human placental membranes and IM-9 lymphocytes. Horm Metab Res 1985;17;328-332.
Wolman SL, Anderson GH, Marliss EB, Jeejeebhoy KN.
Zinc in total parental nutrition: requirements and metabolic effects. Gastroenterology 1979;76:458-467.
Holden IM, Wolf WR, Mertz W.
Zinc and copper in self-selected diets. J Am Diet Assoc 1979;75:23-28.
Sarji KE, Kleinfelder J, Brewington P, Gonzalez J, Hempling H, et al.
Decreased platelet vitamin C in diabetes mellitus: possible role in hyperaggregation. Thromb Res 1979;15:636-650.
Secher K.
The bearing of the ascorbic acid content of the blood on the course of the blood sugar curve. Acta Med Scand 1942;60:255-265.
Verlangieri AJ, Sestito J.
Effect of insulin on ascorbic acid uptake by heart endothelial cells: possible relationship to retinal atherogenesis. Life Sci 1981;29:5-9.
Hutchinson ML, Lee WYL, Chen MS, Davis KA, Ely JTA, et al.
Effects of glucose and select pharmacologic agents on leukocyte ascorbic acid levels. Fed Proc 1983:42:930.
Vinson JA, Staretz ME, Bose P, Kassim HM, Basalyga BS.
In vitro and in vivo reduction of erythrocyte sorbitol by ascorbic acid. Diabetes 1989;38:1036-1041.
Fore H.
Manganese-induced hypoglycemia. Lancet 1963;1:274- 275.
Shrader RE, Everson GJ.
Pancreatic pathology in manganese-deficient guinea pigs. J Nutr 1968;94:269.
Wenlock RW, Buss DH, Dixon EJ.
Trace nutrients. 2. Manganese in British food. Br J Nutr 1979;4 1:253-261.
Wilkinson JF.
Diabetes mellitus and pernicious anemia. Br Med J 1963;1:676-677.
Lifshitz F, Moak SA, Wapnir Ra.
Folic acid in the prevention of fasting induced hypoglycemia. Pediatr Res 1977:11:518.
Haugen HN.
The blood concentration of thiamin in diabetes. Scand J Clin Lab Invest 1964;16;260-266.
Fagin JA, Ikejiri K, Levin SR.
Insulinotropic effects of vanadate. Diabetes 1987;36:1448.
Asayama K, Kooy NW, Burr IM.
Effect of vitamin E deficiency and selenium deficiency on insulin secretory reserve and free radical scavenging systems i isletsz decrease of islet manganosuperoxide dismutase. J Lab Clin Med 1986;107:459-464.
Echert CD, Breskin MW, Wise WW, Knopp RH.
Association between low serum selenium and diminished visual function in diabetic women. Fed Proc 1985;44:1670.
Pennington JAT, Young BE, WiIson DB, Johnson RD, Vanderveer JE.
Mineral content of foods in total diet: selected minerals in food survey. Jour Am Diet Assoc 1986;86:876.
Coggeshall JC, Heggars JP, Robson MC, Baker H.
Biotin status and plasma glucose in diabetics. Ann NY Acad Sci 1985:447:389-393.
Pathological Process related to Metabolic Syndrome by William Beakey, N.M.D.
Foundations of Chinese Medicine by Giovanni Maciocia
Clinical Manual of Oriental Medicine by John Chin
Pathology Illustrated by Churchill Livingstone.
Aging and Reverse Aging by Sang Whang
Biotics Research Seminar on Metabolic Syndrome
Apex Seminar on Pathology and Blood Work

